Most people who have migraine also experience nausea and vomiting during an attack, but what if that connection goes deeper – into the gut? What if there is a link between migraine and gut health and by taking care of your gut you may be able to better manage your migraine?
Some doctors are now saying that is a possibility. In fact, one study has found a strong correlation between migraine and microbes residing in the gut. Additional studies also support the link between migraine and gut health.
Have we been overlooking an important method of migraine treatment? Is there a more effective way to manage attacks? Could we drastically improve migraine by simply taking probiotics and changing our diet?
Not so fast. This research is still in the early stages. There is evidence that good gut health may help improve migraine attacks. However, there is also plenty of evidence that shows taking care of your gut will improve your overall health, so either way, it’s a win.
We talked to Danny Park, M.D., of RevIVe Wellness in the Chicagoland area and Section Head of Neurology at Swedish Covenant Hospital in Chicago to learn more about migraine and gut health.
“Unfortunately, sometimes there are not a lot of studies that look into this,” says Dr. Park. “But there are some and there’s a lot of anecdotal evidence as well. More research definitely needs to be done.”
Here’s the skinny – and what you need to know.

What is gut health?
You have probably heard the term “gut health” and may have even used it in a sentence. But what is it really?
In a nutshell, it is the balance of gut microbiome (gut flora) that reside in the digestive tract. When they are well balanced, good health follows. When there is an imbalance it can cause a number of issues within your body.
There are around 100 trillion microorganisms, called gut microbiota, in your gut. These include viruses, yeasts, and bacteria. Many of these microbes are beneficial for the body and promote good health. There are some that the body requires in order to function at all. However, some of these microbes can be harmful and when they multiply, they can quickly outnumber the “good bacteria” in your gut. That is when things start to go wrong.
Gut microbiota and its role in migraine disease.
It is important to understand the connection between gut microbiota and migraine. Researchers are discovering that while nausea and vomiting often accompany a migraine attack, there’s more going on in the gut than meets the eye. Another study is currently underway exploring this connection. Feng Tao, MD, PhD who is an associate professor at Texas A&M’s College of Dentistry is looking at what happens when the natural routine of gut microbiota is disrupted and results in a migraine attack.
The wheels of progress in this area are turning slowly, but at least there is some motion. Individuals and groups who are in a position to research and find answers are taking migraine very seriously.
“There is more evidence linking the gut with the brain than the more specific migraine disease,” says Dr. Park. “There is a theory that something exists called the gut-brain axis. One influences the other. That’s why most migraine sufferers have GI symptoms as well, including nausea, vomiting, abdominal discomfort, and so on.”
There are other issues involving the gut that can cause migraineurs problems and exacerbate attacks. Dr. Park explains, “Migraine patients can develop a Leaky Gut Syndrome as well. In many cases, this is why typical headache medications may not be helping like they once did. It also adversely affects absorption of nutrients, minerals, and vitamins.”
Because of this snowball effect, it is becoming more and more obvious that medication for migraine may not be enough. One of the most common complaints among migraineurs is that their medication does not work. Dr. Park advised a more whole body approach to treatment.
“It is becoming clearer that we must start treating the whole person,” he says. “This means a multi-faceted approach that includes probiotics, diet changes, IV vitamins and not simply focusing on the brain alone.”

Leaky gut and migraine.
Leaky gut is a common term for a condition called intestinal hyperpermeability or simply intestinal permeability.
The human body is a complex, intricate system. The lower part of the gut, the intestines, have junctions that fit closely together. These junctions control what substances or nutrients are able to pass through the small intestine lining. If those junctions are not working properly, or don’t fit together as they should, it could leave gaps that allow unwanted substances to leak into the bloodstream. When this happens, nutrients may pass through without being absorbed while toxic byproducts from bacteria are absorbed into the body.
Leaky gut is a common problem with Crohn’s disease patients and people who have irritable bowel or celiac disease, but doctors are not certain why it would happen in someone who was healthy or did not have those conditions. In extreme cases, it can lead to vitamin and mineral deficiencies as well as malnutrition.
A large portion of the immune system resides in the gut, so when something isn’t working correctly it can impact the person’s immune response. This leads to inflammation and the entire body can be thrown out of balance. However, inflammation can also cause leaky gut. Because of the inflammation and imbalance, even mild cases can cause a number of health problems, including migraine.
The continuous cycle of gut inflammation and migraine.
So, which came first? Gut inflammation or migraine? Turns out, there isn’t an easy answer for that.
“It’s kind of like the chicken or the egg question,” says Dr. Park. “Migraines are associated with gut inflammation and gut inflammation is associated with migraines.”
It is a vicious cycle that can get you caught in the loop. There are a number of conditions that are associated with gut disease, such as h. pylori, celiac, irritable bowel, gastroparesis, and others. Any of these can be a migraine trigger or have symptoms that trigger migraine. However, a gut disorder does not necessarily mean that the patient will get migraine just as the absence of one does not guarantee they will not have an attack.
There are studies that link migraine to gut inflammation, but there is still much more work to do.

Ensuring good gut health to reduce risk of migraine.
Maintaining a healthy gut may help reduce migraine attacks. According to Dr. Park, it is best to take a two prong approach to good gut health. “Starting a good anti-inflammatory diet as well as a good probiotic are good ways to minimize risks,” he says. “Inflammation in the body can be triggered by inflammation in the gut. During migraines, there is a cascade of neural inflammation that can be mitigated by a healthy GI system.”
This takes a bit of work to put into practice. An anti-inflammatory diet is comprised of foods that reduce or prevent an inflammatory response in the body. The Mediterranean diet is a good example of that. However, for many migraineurs there is such a delicate balance when it comes to triggers, especially in the foods they eat. Adhering to an anti-inflammatory diet or migraine diet is a good start, but some people have found that even certain anti-inflammatory foods are triggers for them.
If food is a trigger, you will have to get creative and make your own diet rich in anti-inflammatory foods. It is important to figure out how your body responds to certain foods and use that information to develop an eating plan that will heal your gut.
Sugar, refined foods, and processed foods are usually the first to go. That works with just about everyone no matter how sensitive they are. Those foods are unhealthy and have been linked to a myriad of health problems. Giving them up is a smart move whether you have migraine or not. It’s when you bring in nutrient rich, whole foods to replace them that problems can arise.
Foods recommended in the diet such as red wine, red grapes, nuts, and dark chocolate may be triggers for some migraineurs. This means that they will have to find good, healthy alternatives. Fortunately, the list of anti-inflammatory foods is rather extensive. There should be no problem finding substitutions.
Choosing a “good” probiotic.
Taking a probiotic supplement will help increase the beneficial bacteria in your gut. You may have seen them on store shelves, but it is important to keep in mind that not all probiotics are the same.
You can find probiotics at drug stores, grocery stores, health foods stores, and even online. However, some probiotics are better than others. Don’t just purchase the first one you see or buy the one that is the cheapest. Take your time and find a good probiotic that will give you what you need. Otherwise, you are just wasting your time and money.
“I typically recommend a probiotic that is refrigerated and has bifido,” says Dr. Park. “In addition, looking into prebiotics and a healthy anti-inflammatory diet will help.”
When you are looking for a probiotic, follow these tips:
- Shop for a brand that you trust.
- Get the right type of probiotic to treat your issue.
- Get the right CFUs for your condition
- Pay attention to how you should store it (refrigerate or not)
- Check the “other ingredients” to make sure there is nothing that that could be a trigger.

Therapies and treatments that promote gut friendly practices.
Often, when it comes to migraine and gut health, working on one helps the other. For instance, improving your gut health for IBS will often have far reaching benefits such as increased energy, a healthier heart, and fewer migraines.
Good gut health requires a whole body approach. Just changing your diet is not enough. You need to take care of your whole body in order to reap the full benefits.
“If someone is having worsening migraines, that is a sign for me that their body is out of balance,” says Dr. Park. “They likely have increased GI inflammation with the leaky gut syndrome I spoke of earlier. This in turn limits the GI system’s ability to absorb nutrients, minerals, and vitamins. I therefore recommend IV vitamin/mineral supplementation, probiotics, and a re-evaluation of the diet. In addition, you need to make sure you’re sleeping well, exercising daily, and addressing other psychological factors, including stress/depression/anxiety, with mental health treatments or meditation, yoga, and so on.”
Incorporating fermented foods like tempeh, kefir, sauerkraut, kimchi, and others will also help improve gut health. Fermented foods are natural probiotics.
Some research has shown that eating foods rich in prebiotics also helps improve gut health. Bananas, garlic, asparagus, onion, and whole grains are all very high in prebiotics and are worth including in your diet.
Migraine and gut health – what to expect when you take action.
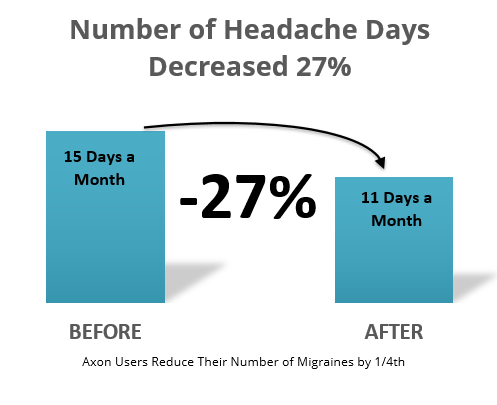
Once you decide to start working on your gut, you will probably want to see results quickly. The truth is, some people notice a difference within a few days, but most people don’t feel the full effects of a probiotic until they have taken it for about a month. That’s how long you should give it in order to determine whether it is working for you or if you need to try something else.
Most probiotics do not cause any real side effects although some people may experience a little more gassiness than usual.
“Everyone’s response is different,” says Dr. Park. “I’ve had some patients who simply cut out gluten from their diet and they improved within 1-2 weeks. I have also had some patients who focused on their mental health, and they improved within several weeks to a couple months. I do not think there is a magic treatment. It takes a combination of different treatments, including anti-inflammatory diet, probiotic, iv vitamins, exercise, sleep, mental health, etc. And sometimes traditional medications play a role as well.”
As your gut heals, you may notice that you sleep better, have more energy, move easier, and your memory is better. You may feel more positive or happier as well. As your body comes back into balance and you remain consistent with your diet, you should notice overall good, well feelings.
Dr. Park says, “Starting an anti-inflammatory diet typically does not cause any side effects; however, if you slip and eat a type of food that causes GI inflammation, it can cause abdominal discomfort, bloating, loose stool, and nausea and/or vomiting.”
Moral of the story, don’t “slip up” and eat something that will cause inflammation. It isn’t worth it.
Dr. Park believes that having a combination of treatments is the best course of action.
“Traditional medicine can help,” he says. “But I do not think it’s enough. You cannot solely focus on the head. If you do, you may not succeed. All parts of the body are connected.”
The connection between migraine and gut health is compelling, but it is still in its infancy. What we do know is that lifestyle changes can help both conditions improve, but consistency is key. This means that the anti-inflammatory diet is just the tip of the iceberg. You also have to get enough sleep, exercise, and learn how to manage your stress. Wearing migraine glasses can help reduce stress on your body by decreasing the effects of light sensitivity which can be a migraine trigger.
Be good to your body; it’s the only one you have.

Resources
Danny Park, M.D.
Section Head of Neurology at Swedish Covenant Hospital
Chicago, IL
RevIVe Wellness in the Chicagoland area
Cutler, Nikki. “Gut-Brain Axis: RCT Shows Gut-Friendly Probiotic Improves Migraine Symptoms.” Nutraingredients.com, William Reed Business Media Ltd., 30 Jan. 2019, www.nutraingredients.com/Article/2019/01/30/Gut-brain-axis-RCT-shows-gut-friendly-probiotic-improves-migraine-symptoms.
Cámara-Lemarroy, Carlos R, et al. “Gastrointestinal Disorders Associated with Migraine: A Comprehensive Review.” World Journal of Gastroenterology, Baishideng Publishing Group Inc, 28 Sept. 2016, www.ncbi.nlm.nih.gov/pmc/articles/PMC5037083/.
Gonzalez, Antonio, et al. “Migraines Are Correlated with Higher Levels of Nitrate-, Nitrite-, and Nitric Oxide-Reducing Oral Microbes in the American Gut Project Cohort.” MSystems, American Society for Microbiology Journals, 25 Oct. 2016, msystems.asm.org/content/1/5/e00105-16.
Hindiyeh, Nada, and Sheena K. Aurora. “What the Gut Can Teach Us About Migraine.” SpringerLink, Springer US, 7 June 2015, link.springer.com/article/10.1007/s11916-015-0501-4.
Jerry W. Swanson, M.D. “The Link between Migraines and Gut Problems.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 10 May 2019, www.mayoclinic.org/diseases-conditions/migraine-headache/expert-answers/migraines/faq-20058268.
McMillen, Matt. “Defining Leaky Gut Syndrome: Common Symptoms and the Difficulty of Diagnosis.” WebMD, WebMD, 14 Aug. 2013, www.webmd.com/digestive-disorders/features/leaky-gut-syndrome#1.
Preidt, Robert. “Mouth and Gut Germs May Be Linked to Migraines.” WebMD, WebMD, 18 Oct. 2016, www.webmd.com/migraines-headaches/news/20161018/mouth-and-gut-germs-may-be-linked-to-migraines.
Revelant, Julie. “Migraines and Fatigue May Start in the Gut, Experts Say.” Fox News, FOX News Network, 16 June 2016, www.foxnews.com/health/migraines-and-fatigue-may-start-in-the-gut-experts-say.
UVM Medical Center. “Migraine and the Gut Microbiome.” UVM Medical Center Blog, 17 July 2018, medcenterblog.uvmhealth.org/brain-nervous-system/migraine-gut-microbiome/.
Van Hemert, Saskia, et al. “Migraine Associated with Gastrointestinal Disorders: Review of the Literature and Clinical Implications.” Frontiers in Neurology, Frontiers Media S.A., 21 Nov. 2014, www.ncbi.nlm.nih.gov/pmc/articles/PMC4240046/.