Over 90% of migraine sufferers are sensitive to light. During a migraine attack, sufferers are bothered by light and prefer to be in a dark room. Migraineurs are particularly sensitive to non-incandescent indoor lighting sources such as fluorescent lights, computer monitors, LEDs, and gas-vapor lamps.
Migraine Sufferers Report Light Sensitivity
Although nearly all migraine sufferers report light sensitivity (photophobia) during attacks, and many report that light can trigger an attack, there are no treatments that specifically address this facet of this disease.
Ocular Migraine or “Migraine with Aura”
About a third of the migraine sufferers in the U.S. experience migraine with aura. Of course, everyone is different, and symptoms vary by person and sometimes by attack. These migraines are believed to be caused by the same stimuli as a normal migraine headache, but the symptoms vary. Symptoms may come in the form of enlarging blind spot, wavy or zig-zag lines surrounding the blind spot, and other vision impairments. Often these migraines are painless and will resolve without medication in 20 to 30 minutes.
Learn more about migraines with aura
The Science behind Light Sensitivity
The physiological basis of light sensitivity has always been a mystery: Why is it that when one looks at a bright light, such as the sun, one feels pain? Why can light trigger a painful migraine attack? What part of the eye transforms light into a painful stimulus?
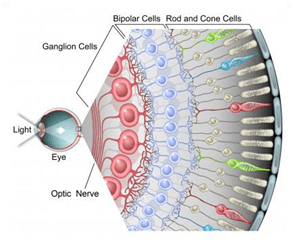
Many parts of the eye work together to transform light rays passing through your pupil into images that your brain can interpret. The retina is the very back of the eye and holds millions of cells that are sensitive to light. The retina takes the light the eye receives and converts it into electrical signals so the brain can interpret what the eye is seeing.
Light Sensitivity Can Produce Pain
However, research performed in 2010 by Harvard and University of Utah scientists suggest that an additional pathway between the eye and brain exists that does not produce images – it may produce pain. In the early 1990’s, a unique subset of cells in the retina were found to be intrinsically sensitive to light.
It is likely that the pain pathway begins with these intrinsically light sensitive cells and can transform light absorbed by the eye into a painful stimulus. This pain pathway is completely separate from and independent of the image-forming pathway. Because it is a separate pathway, even some profoundly blind patients can be profoundly light sensitive.
References
1 Source: Evans RW, Seifert T, Kailasam J, Mathew NT. The use of questions to determine the presence of photophobia and phonophobia during migraine. Headache 2008;48:395-7. http://www.ncbi.nlm.nih.gov/pubmed/17868350
2 Source: Main A, Dowson A, Gross M. Photophobia and phonophobia in migraineurs between attacks. Headache. 1997. 37:492-5. http://www.ncbi.nlm.nih.gov/pubmed/9329231
3 Source: Cortical spreading depression—Migraine: a complex genetic disorder; Lancet Neurology, Wessman, 2007 http://www.ncbi.nlm.nih.gov/pubmed/8800932
4 Source: Noseda R, Kainz V, Jakubowski M, Gooley JJ, Saper CB, Digre K, Burstein R. A neural mechanism for exacerbation of headache by light. Nat Neurosci. 2010. 13:239-45.http://www.ncbi.nlm.nih.gov/pubmed/20062053
5 Source: Güler AD, Ecker JL, Lall GS, et al. Melanopsin cells are the principal conduits for rod-cone input to non-image-forming vision. Nature. 2008. 453:102-5. http://www.ncbi.nlm.nih.gov/pubmed/18432195
6 Source: Amini A, Digre K, Couldwell WT. Photophobia in a blind patient: An alternate visual pathway. Case report. J Neurosurg. 2006. 105:765-8. http://www.ncbi.nlm.nih.gov/pubmed/17121141