You have a headache. It extends over your eye and you have pressure in your face. Your nose even runs a little. You take a decongestant or ibuprofen, tell everyone you have a sinus headache or even a sinus migraine, and lay down for a while. Two or three hours later you are better. You might have a little residual soreness and you might be a little tired, but the worst of the headache is over. You’ve just had a sinus headache – or was it?
You could have had a migraine that isn’t even related to any sinus issues and not realize it. You felt sinus pain and pressure, so your mind automatically went to sinus headache. Your doctor may even have told you it was sinus related and the subject of migraines never came up. It happens a lot more than you might think. In fact, nearly 90% of patients who visit their doctor and complain of “sinus headache” actually have a migraine or migraine-type headache.
This is an easy misdiagnosis, but it's important to get it right because sinus-related headaches and straight-up migraines are treated differently. For a sinus headache, a decongestant could be key. But if you're having a migraine, you might benefit most from a pair of migraine glasses like these, or other remedies that are designed for migraine.

Some people call it a “sinus migraine” because the symptoms so closely resemble a sinus headache. “Allergy migraine” is another common term. However, researchers have found that there are distinct differences between a migraine and a sinus headache. In fact, some doctors say that the headaches that many people believe are related to sinus issues are actually migraines.
Axon Optics talked to Dr. Jessica Ailani, Director of Medstar Georgetown Headache Center and Associate Professor of Neurology at Medstar Georgetown University Hospital about sinus migraine versus sinus headaches. She says, “Often, patients with a headache disorder will have seen their primary care physician (PCP) and been treated for a sinus infection, then referred to both an ear, nose, and throat doctor (ENT) and an Ophthalmologist before they eventually make their way to a Neurologist. One of the reasons for this is that a number of headache disorders, including migraine, can have symptoms very similar to sinus problems.”
Is There Really a “Sinus Migraine”?
Technically, the answer is no. There are migraines and there are sinus headaches. They are not the same, but some people have coined the phrase “sinus migraine” to make the distinction that their migraines seem to have a sinus component. They may be familiar enough with migraines that they know the typical symptoms, so they rule it out because their headaches don’t fit that mold. The truth is, there are many different types of migraines and headaches – and they often have very similar, if not identical, symptoms.
Dr. Ailani explains, “Migraine pain can be located in the temples or back of the head, but often is in or around the eye and can, on occasion, be located under the eye, around the nose, and into the jaw. The reason for this is that the nerve that causes facial sensation and sinus sensation and the one that also causes facial and sinus pain, are one and the same, the trigeminal nerve.”
She continues, “When this nerve is turned on, you can experience pain- which can be all different types such as pulsating, throbbing, pressure, searing, jabbing, tingling, and burning, anywhere in your head and face. This nerve also connects to other nerves at the back of the neck and in the sinuses. When one nerve decides to be turned on, other connected nerves can follow- where there is a party, all like to join in!”
Many people mistake this migraine activity to be a sinus headache or sinus migraine, then become frustrated when their sinus medication doesn’t help their pain (although sometimes it can). Understanding the differences between the two can help you manage your headaches better and it could even help you prevent them altogether.

Sinusitis and Sinus Headaches
What most people don’t realize is that true sinus headaches are actually quite uncommon and are often over diagnosed or misdiagnosed. Sinusitis is an inflammation of the sinuses, often due to a bacterial infection. The sinuses are air pockets that are situated at certain points in the facial bones. Scientists are not certain the exact purpose of sinuses. Some believe that it helps enhance the voice through resonation while others believe it may be a way for the body to humidify the air during inhalation. They are usually empty but do have a very thin mucus layer along the walls.
There are four pairs of paranasal sinuses,
meaning that there are two at the same points on the left and right.
They are:
- Frontal sinuses: above the eyes just over the eyebrows
- Maxillary sinuses: on each side of the nose, in the cheekbone
- Ethmoid sinuses: between the eyes, under the bridge of the nose
- Sphenoid sinuses: behind the eyes and ethmoid sinuses
Inflammation of the sinuses can occur due to bacterial, viral, or fungal causes and can present in one of the sinus pair, or several. If there is an infection present, it is important that it is treated. Failure to properly treat a sinus infection can cause serious health risks and can create a propensity to develop sinus infections in the future.
Can a Sinus Headache Cause a Migraine?
A common misconception is that sinusitis triggers migraines (hence the term sinus migraine), but that isn’t likely to happen. Sinusitis originates in a different region of the body than migraine and they are not necessarily connected However, the two conditions do share the same nerves that can be stimulated, and they do both produce many of the same chemicals in the body during an attack. There are certain signs that can help distinguish between the two and knowing this can help facilitate appropriate treatment of the condition that is present.
Dr. Ailani explains how easy it can be to mistake a migraine for a sinus headache:
“With a sinus infection, you will often have a fever, bright colored mucus from the nose in large amounts, and pain that is worse when you lay down (as the fluid collects into your sinuses). You may notice the pain is worse in the morning after sleeping for several hours. Occasionally, someone may have a chronic sinus infection, something that has been going on for several months. In this case, a person may not have any symptoms, and may not have a headache either.
If you have a severe headache with sinus type symptoms (like congestion, eye-watering) and also have light or sound sensitivity, upset stomach, lack of appetite, and no fever, and you notice the pain resolves in 4-36 hours - this may be a migraine. If you notice the pain improves when laying in a dark, quiet room, or when taking over the counter pain medication, this again goes along with migraine.”
Tension headaches are also often mistaken for sinus headaches. Interestingly, tension headaches are often misdiagnosed as well, but tension can also bring on a migraine attack. All of these conditions are so much alike it can delay an accurate diagnosis or prevent it altogether.
Migraine vs Sinus Headache
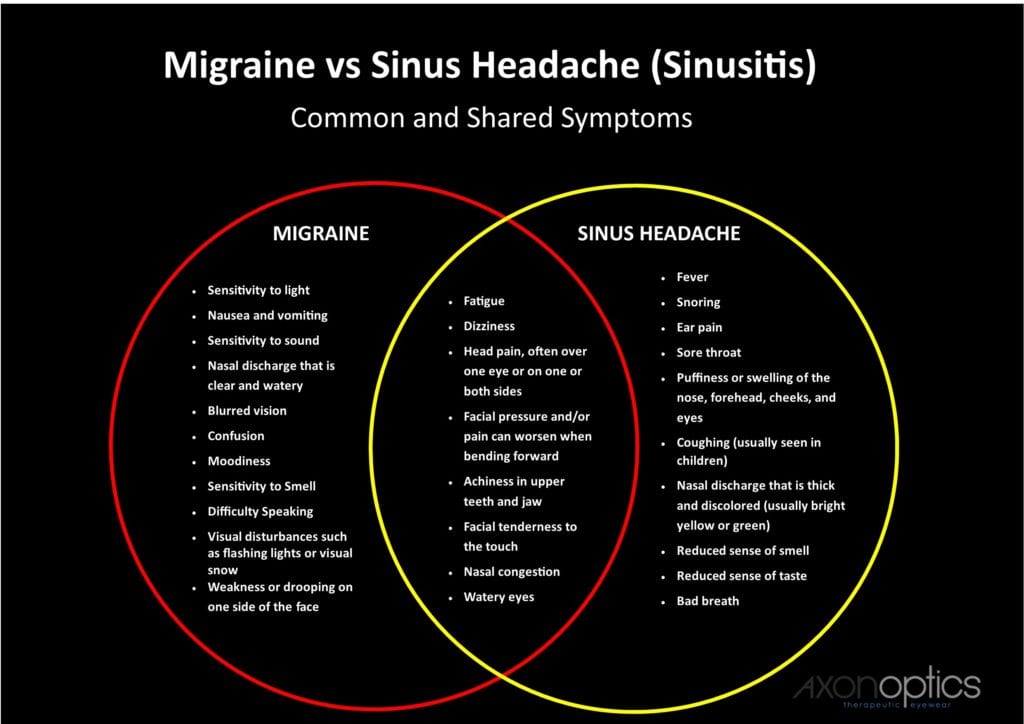
It isn’t always easy to tell the difference between a migraine and a headache, much less a sinus headache, but each condition does have its own set of specific symptoms. While some are shared, others are very distinct to the condition. This creates a strong case for keeping a migraine diary and documenting the details of and surrounding your headaches.
According to Dr. Ailani, the symptoms of migraine and sinus headache are similar because of the region of the brain that is activated during an attack:
“Migraine can also have associated symptoms, symptoms that come WITH the headache pain that can be confused for a sinus or allergy problem. You can have a runny nose, watery eyes, your eyes can turn red. These symptoms, called autonomic symptoms, come on because of the area in the brain, the hypothalamus, that gets turned on during migraine.”
Following this section are common symptoms for migraines as well as sinus migraine, sinus headaches and sinusitis. As you can see, many of them are identical or nearly identical. It’s no wonder that patients struggle to describe their head pain and doctors struggle to diagnose it. The problem is, without a proper diagnosis you can’t get proper treatment. If you are diagnosed with sinus headaches but you actually have migraines, it could delay your migraine treatment for years.
Symptoms of a Migraine
Migraines can vary from person to person and even from attack to attack. There are a wide range of migraine symptoms, but the most common include:
- Head pain, often over one eye or on one or both sides
- Sensitivity to light (photophobia)
- Nausea and vomiting
- Facial pressure (pressure and/or pain can worsen when bending forward)
- Facial tenderness to the touch
- Sensitivity to sound (phonophobia)
- Fatigue
- Visual disturbances such as flashing lights or visual snow
- Nasal congestion
- Nasal discharge that is clear and watery
- Watery eyes
Symptoms of a Sinus Headache and Sinusitis
Sinusitis and sinus headaches share many of the migraine symptoms, except for photophobia, nausea, vomiting, and phonophobia. These symptoms are almost always exclusive to migraines in these cases. Symptoms of a sinus headache and sinusitis include:
- Head pain behind the eyes or on one or both sides including the forehead, nose, and cheeks
- Fever
- Sore throat
- Achiness in upper teeth and jaw
- Fatigue
- Tenderness and puffiness or swelling of the forehead, nose, cheeks, and eyes
- Nasal congestion or stuffiness (can include varying degrees of obstruction from partial to total)
- Difficulty breathing through the nose
- Nasal discharge that is thick and discolored (usually bright yellow or green)
- Sense of smell is reduced as well as sense of taste
- Bad breath
- Snoring
- Ear pain
- Coughing (especially in children)
To further compound the confusion between these two conditions, even treatment options are similar. Many people are very surprised to discover that sinus medications and treatments relieve their migraine pain. Dr. Ailani explains:
“Migraine can improve when using products like Sudafed or Advil cold/sinus. These medications work to reduce some of the chemicals that are elevated during a migraine, so don’t be fooled into thinking that if you feel better with Sudafed, it is a sinus issue. Overuse of these medications can lead to more headaches, so if you find yourself using these medications more than 2-3 days a week, seek medical attention for an appropriate diagnosis.”
A diagnosis of either a migraine or a sinus headache is the first step in finding treatment that works.

Getting a Diagnosis
Diagnosing migraines is not an exact science and determining the difference between migraines and sinus headaches isn’t always easy. You can’t take a blood test or get an x-ray to see the problem, although if you are fighting a sinus infection, your bloodwork may show an elevated white blood cell count. It usually takes a great deal of documentation and probably several doctors’ visits – sometimes even visits to specialists – before a migraine diagnosis can be made.
Sinusitis is a little easier to diagnose, but if a headache accompanies what appears to be sinus symptoms, the matter becomes much more complex and difficult. Most people begin the journey by going to their primary care doctor when they have headaches – and there is nothing wrong with that. They may be able to help. However, sometimes it is necessary to see a doctor who specializes in headaches related issues.
Dr. Ailani recommends seeing a specialist if your headaches are frequent or resistant to treatment. She says, “If you are experiencing frequent headaches and find you are either not responding to medication options over-the-counter or given to you by your provider, or taking these options too frequently, consider seeing a Neurologist or Headache specialist for your symptoms to confirm your diagnosis and find better options for your headaches.”
A migraine diagnosis requires some detective work and other conditions must be ruled out before it can be officially made. The doctor will evaluate your symptoms and review your family’s medical history as well as yours. They will look for potentially inherited conditions as well as patterns in your health. They will rule out other conditions with diagnostic tests including bloodwork, x-rays, CAT scans, and MRIs. If you have been keeping a headache diary, they will review your headache history, looking for patterns in triggers, frequency, and characteristics of the headaches. The migraine is diagnosed once other conditions are ruled out and your symptoms support it.
If you have symptoms of sinusitis, you may be referred to an ENT in order to rule out sinus issues as a cause of your headaches or to identify any underlying problems. If your doctor determines that you have a sinus issue, then they will address it and treat it appropriately.
Treatment for Migraines
There is no known cure for migraines and many migraineurs struggle to find a treatment that works. There is a lot of research currently underway as doctors and scientists continually seek effective relief options. Migraine medications tend to be expensive though, so some people turn to natural migraine remedies. Other options include migraine release surgery, Botox injections, and electrical and magnetic stimulators. Light sensitivity is the number one most bothersome migraine symptom, according to the 2019 MAST study. It's important you also use a light management tool like these migraine glasses.
“Migraines with symptoms similar to sinus pain or pressure are not treated any differently than migraines without those symptoms,” says Dr. Ailani. “For attacks of migraine, we use what are called acute therapies. These are medications you take at the start of the attack to improve pain and associated symptoms. Medications range from over the counter options, like acetaminophen and ibuprofen for milder attacks, to prescription medications for more moderate to severe attacks, or fast onset attacks.”
She continues, “The most commonly prescribed migraine specific acute medications are in a category called triptans. They are designed to specifically reduce certain chemicals in the brain that are out of control during a migraine attack. They come in pill form, nasal forms, and injections, to help match your symptom need. For example, if you feel nauseated during a migraine, swallowing a pill can be hard, so using a nasal form may be preferred. If you wake with a severe migraine or are vomiting, an injectable form may be preferred.”
She concludes, “If you are having frequent migraines, meaning you have them more than 1 day a week, or the migraine attacks are disabling, you may be a candidate for preventive treatment. This is the use of medication daily to reduce the frequency of migraine attacks, allowing you to use less acute medication and improve daily functioning. There are a variety of preventive treatments, so it is best to see a provider to find out what option is best for you.”

Treatment for Sinusitis and Sinus Headaches
Some aspects of the treatment for sinusitis and sinus headache (or sinus migraine) are not all that different from migraine treatments. The treatment goals are:
- To reduce inflammation
- To facilitate drainage of the nasal passages
- To identify any underlying causes and eliminate them
- In the case of chronic sinusitis, reduce the number of attacks or flare-ups
These are very similar to migraine treatment goals: reduce the pain of the attack, facilitate the treatment of comorbidities or symptoms that compound the discomfort, identify any triggers and eliminate them, and in the case of chronic migraine, reduce the number of attacks.
Sinusitis treatments include a combination of symptom relief and addressing the cause. They may include:
- Oral, nasal, or injected corticosteroids
- Saline nasal irrigation
- Warm compresses applied to the face
- Moisturizing nasal spray
- Steam treatment
- Aspirin desensitization treatment
- Acetaminophen or ibuprofen for fever and pain
- Antihistamines (prescription or over the counter)
- Antibiotics (if the cause is bacterial)
- Environmental changes such as a humidifier or dehumidifier in the home
- Immunotherapy
- Surgery
In cases where a sinus migraine or sinus headache is present, treating the symptoms and condition will usually relieve the headache.
Talking to Your Doctor About Your Headaches
Your search for a migraine diagnosis and relief from your headaches usually begins with your primary care provider. He or she may send you to several specialists before you get answers, or you may go directly to a headache specialist or neurologist. In other words, you may find that you are repeating yourself to each new doctor. Don’t let this discourage you. Sometimes it takes a little digging and searching to get answers, but it is worth it. Create your own headache file with notes and documentation from doctors’ visits and tests as well as your migraine diary.
Dr. Ailani has this advice: “Keep track of your headaches, write down when they happen, how long they last, and what symptoms come with the headache.”
She also recommends noting specific characteristics of your headache or migraine by considering these questions:
- Do you prefer to be in the dark, or in a quiet area with a headache?
- Do you find your stomach gets upset and smells bother you?
- Would you prefer to sleep if you could?
- Do your headaches last several hours or several days?
- Have your parents, siblings, aunts/uncles, grandparents, and cousins ever had headaches? Migraines tend to run in families, but most families don’t discuss this.
- What have you tried for your headaches? What works or does not work?
- How have your headaches changed over time?
Dr. Ailani stresses that this is the best way to approach your search for a diagnosis from the very start. “Bring this information to your primary care provider to discuss and ask for advice on how to better manage headaches,”
She says that if you don’t respond to the first step treatments, you may then be referred to a Neurologist or headache specialist for further diagnosis and management. Getting a diagnosis may not be as simple and straightforward as we’d all like, but once you get it, you can begin moving towards getting relief.

Allergy, Sinusitis, and Sinus Headache Resources
There are a number of very good resources available for people suffering from allergies, sinusitis, and sinus headaches:
- Patient.info Sinusitis Forum Discussion
- Patient.info Allergic Disorders Allergic Discussion
- eHealth Forum Sinusitis Forum
- Chronic Sinusitis Sufferers Facebook Group
- Chronic Sinusitis Support Group
Migraineurs can use the search feature on the Axon Optics blog to find information on specific migraine types, migraine treatments, tips for coping with migraine related issues like light sensitivity, and much more.
References and Resources (Yes, we did our homework): The information in this article is based on an interview with Jessica Ailani M.D. who is the Director of the Medstar Georgetown Headache Center and Associate Professor of Neurology at Georgetown University Hospital. Additional info came from over 15 references including Dr. Goadsby’s article from The Journal of Headache and Pain.
References
-
Jessica Ailani M.D. FAHS
Director, Medstar Georgetown Headache Center
Associate Professor Neurology
Department of Neurology
Medstar Georgetown University Hospital
https://www.medstarhealth.org/doctor/dr-jessica-ailani-md/ - Al-Hashel, J. Y., Ahmed, S. F., Alroughani, R., & Goadsby, P. J. (2013, December 12). Migraine misdiagnosis as a sinusitis, a delay that can last for many years. Retrieved from https://thejournalofheadacheandpain.springeropen.com/articles/10.1186/1129-2377-14-97
- Bono, F., Messina, D., Giliberto, C., Cristiano, D., Broussard, G., Fera, F., . . . Quattrone, A. (2006, August 08). Bilateral transverse sinus stenosis predicts IIH without papilledema in patients with migraine. Retrieved from http://n.neurology.org/content/67/3/419.short
- Cady, R. K., & Schreiber, C. P. (2002, May 14). Sinus headache or migraine? Retrieved from http://n.neurology.org/content/58/9_suppl_6/S10.short
- Chronic sinusitis. (2016, July 01). Retrieved from https://www.mayoclinic.org/diseases-conditions/chronic-sinusitis/symptoms-causes/syc-20351661
- C. (2018, January 03). Sinus Headaches. Retrieved from http://www.entnet.org/content/sinus-headaches
- December;62(12):752-754, J. F., & Author(s): Christopher Boisselle, MD Richard Guthmann, MD, MPH Kathy Cable, MLS. (2016, December 13). What clinical clues differentiate migraine from sinus headaches? Retrieved from https://www.mdedge.com/jfponline/article/79122/pain/what-clinical-clues-differentiate-migraine-sinus-headaches
- Diamond, M. L. (2002, May 14). The role of concomitant headache types and non-headache co-morbidities in the underdiagnosis of migraine. Retrieved from http://n.neurology.org/content/58/9_suppl_6/S3.short
- ENT Health. (2018, August). Sinus Headaches. https://www.enthealth.org/conditions/sinus-headaches/
- Eross, E., Dodick, D., & Eross, M. (2007, February). The Sinus, Allergy and Migraine Study (SAMS). Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/17300361
- Eross, E., Dodick, D., & Eross, M. (2007, February 13). The Sinus, Allergy and Migraine Study (SAMS). Retrieved from http://onlinelibrary.wiley.com/doi/10.1111/j.1526-4610.2006.00688.x/full
- Jones, N. S. (2009, April). Sinus headaches: Avoiding over- and mis-diagnosis. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/19344297
- Migraine Symptoms. (n.d.). Retrieved from http://www.axonoptics.com/migraine-symptoms/
- Optics, A. (2016, October 04). Headache or Migraine? How You Know the Difference. Retrieved from http://www.axonoptics.com/2016/09/headache-migraine-know-difference/
- Optics, A. (2017, December 27). Natural Migraine Remedies: A Comprehensive Guide. Retrieved from http://www.axonoptics.com/2017/11/natural-migraine-remedies/
- Optics, A. (2018, February 28). Visual Snow Guide | Everything You Wanted to Know About Visual Snow. Retrieved from http://www.axonoptics.com/2017/03/visual-snow-guide/
- Optics, A. (2017, November 17). What Migraine Medications are Available to Me? Retrieved from http://www.axonoptics.com/2017/08/migraine_medications_available/
- Schreiber, C. P., Hutchinson, S., Webster, C. J., Ames, M., Richardson, M. S., & Powers, C. (2004, September 13). Prevalence of migraine in patients with a history of self-reported or physician-diagnosed “sinus” headache. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/15364670
- Schreiber, C. P. (2004, September 13). Prevalence of Migraine in Patients With a History of Self-reported or Physician-Diagnosed “Sinus” Headache. Retrieved from https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/217302
- Sinus Headaches. (n.d.). Retrieved from https://www.fauquierent.net/sinusheadache.htm
- Sinus headaches. (2015, March 18). Retrieved from https://www.mayoclinic.org/diseases-conditions/sinus-headaches/symptoms-causes/syc-20377580
- Types of Headaches Guide. (n.d.). Retrieved from http://www.axonoptics.com/types-of-headache-guide/
- US8676330B2 – Electrical and magnetic stimulators used to treat migraine/sinus headache and comorbid disorders. (n.d.). Retrieved from https://patents.google.com/patent/US8676330B2/en
- Sinusitis. (n.d.). Retrieved from https://medical-dictionary.thefreedictionary.com/sinusitis